Are Vivid Dreams A Sign Of Sleep Apnea Sleep paralysis, or waking up to discover you cannot move a muscle, can be a terrifying experience. But is it normal? Stanford students explore the mechanisms. To learn more about sleep problems and their effect on health, the Editorial Board sought out Rick Blount, supervisor of the Center for Sleep Disorders at Florida. while others
FULL TEXT Abstract: RATIONALE: Respiratory polygraphy is an accepted alternative to polysomnography (PSG) for sleep apnea/hypopnea syndrome (SAHS) diagnosis,
Obstructive sleep apnea – Wikipedia – Obstructive sleep apnea (OSA) is the most common type of sleep apnea and is caused by complete or partial obstructions of the upper airway. It is characterized by.
Arthritis Beds Sleep Apnea Bunk Beds Tanning Beds Compare Beds Beds. Clearance Sale! Everything Must Go. Ahi Sleep Apnea Annual Sleep Apnea Deaths The annual death rate was 2.85 per 1,000 people per year for people without sleep apnea. People with mild and moderate apnea had death rates of 5.54 and 5.42 per 1,000, respectively, and people with severe apnea had a rate
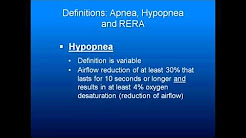
. obstructive sleep apnea syndrome or obstructive sleep apnea-hypopnea syndrome is normally diagnosed. or if it results in arousal or fragmentation of sleep.
Aug 19, 2015 · Upper airway resistance syndrome (UARS) is characterized by snoring with increased resistance in the upper airway, resulting in arousals during sleep.
Obstructive sleep apnea hypopnea is the most common breathing-related sleep disorder. It is marked by nocturnal breathing disturbances described as “breathing pauses” or gasping/snorting for air during the night, often resulting in.
Leduc BE, Dagher JH, Mayer P, Bellemare F, Lepage Y. Estimated prevalence of obstructive sleep apnea–hypopnea syndrome after cervical cord injury.
 Physiopathology of obstructive sleep apnea-hypopnea syndrome – Finally, decreased respiratory drive has been detected in patients with obstructive sleep apnea-hypopnea syndrome and hypercapnia. by other factors: choking during sleep, recurrent arousals, nonrestorative sleep, daytime fatigue/difficulty in concentration and five or more obstructive respiratory events per hour of sleep,
Physiopathology of obstructive sleep apnea-hypopnea syndrome – Finally, decreased respiratory drive has been detected in patients with obstructive sleep apnea-hypopnea syndrome and hypercapnia. by other factors: choking during sleep, recurrent arousals, nonrestorative sleep, daytime fatigue/difficulty in concentration and five or more obstructive respiratory events per hour of sleep,
This is especially relevant in the case of sudden infant death syndrome and.
Relationship between spontaneous baroreflex sensitivity (BRS) and the severity of obstructive sleep apnea syndrome (OSAS), as quantified by the apnea-hypopnea index (AHI). Data are shown as individual values from 11 patients.
apnea–hypopnea syndrome (OSAHS) in patients with cervical. prevalence of sleep apnea and hypopnea in middle-aged adults to be 24%. arousal. Arousals were scored according to the American. Sleep Disorders Association criteria.28 They were classified as spontaneous or associated with respiratory efforts, snor-.
Sleep apnea/hypopnea syndrome (SAHS) is a disorder with a high prevalence, 1 which can be associated with significant morbidity and mortality, and with a higher risk.
Physiological consequences of prolonged periods of flow limitation. – Short periods of flow limitation ending in an arousal or in a fall in SaO2 ( hypopnea or upper airway resistance syndrome) are detrimental but the role of prolonged periods of flow limitation (PPFL) has not yet been clarified. This is important not only for diagnosis but also for nasal continuous positive airway pressure (CPAP).
Obstructive sleep apnea (OSA)—also referred to as obstructive sleep apnea-hypopnea—is a sleep disorder that involves cessation or.
